pediatric septic arthritis
- related: Pediatric
Septic arthritis is a joint infection that frequently involves the hip or knee in young children. Most cases occur in healthy children, but patients with immunodeficiencies, prior joint surgery, hemoglobinopathies, juvenile idiopathic arthritis, and diabetes mellitus are at increased risk.
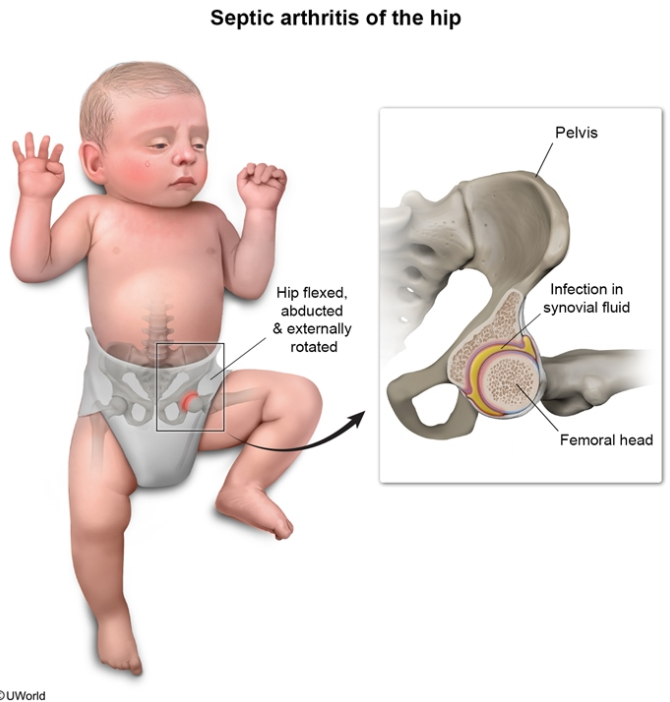
Patients with septic arthritis of the hip usually have swelling and decreased range of motion around the joint. Children often keep the hip in a flexed, abducted, and externally rotated position. In children with unilateral hip pain, septic arthritis can be differentiated from other etiologies, such as transient synovitis (post-viral inflammatory reaction of the joint), based on the following criteria (ie, Kocher criteria):
- Non–weight-bearing
- Fever ≥38.5 C (101.3 F)
- Erythrocyte sedimentation rate >40 mm/hr OR C-reactive protein >2.0 mg/dL
- Leukocytosis
Pediatric patients with ≥3 criteria have a high likelihood of septic arthritis (>93%), and immediate joint aspiration is performed to both establish the diagnosis and decompress the joint. Once the diagnosis is confirmed, empiric parenteral antibiotics as well as surgical drainage and debridement of the joint are required. A delay in diagnosis and treatment can result in joint damage, avascular necrosis, femoral head enlargement, and limb length discrepancy.
- Age <3 months: Staphylococcus aureus, group B Streptococcus, gram-negative bacilli
- Age ≥3 months: Staphylococcus aureus, group A Streptococcus
Staphylococcus aureus, followed by Streptococcus pneumoniae and S pyogenes, is the most common pathogen causing septic arthritis in all ages. Empiric coverage for Staphylococcus aureus and streptococci with an agent such as vancomycin is required. Group B Streptococcus and gram-negative bacilli are also common pathogens in infants age <3 months, in whom vancomycin plus cefotaxime is indicated.